An AI-powered app aimed to help construction workers experiencing anxiety, depression, and suicidal thoughts netted a first place win at the first inaugural John E. Martin Healthcare Tech Challenge. The competition was held online Nov. 16-20.
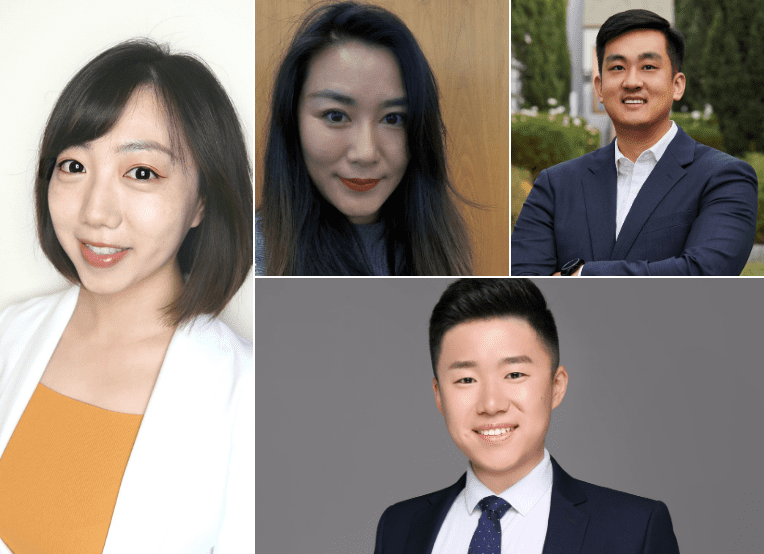
The winning team, Team CLiKS, included Eugene Kim, Zhuoran Li, Zixuan Chen, and Chen Su, all EWMBA 23. The team competed against 11 other teams from top U.S. business schools, including Wharton, Harvard, Columbia, MIT Sloan, and Kellogg for $10,000 in prize money.
Another Haas team placed second, earning $4,000 in prize money for pitching a chatbot that could collect health data, such as sleep patterns and appetite, and recommend tele-health therapy and wellness ambassadors stationed at construction worksites.

Team members included Sophie Schonfeld, Ben Delikat, both MBA/MPH 21; Doug Pollack, MBA/MPH 20; and Vishalli Loomba, MD/MS 23.
The competition was organized by the Berkeley Haas Healthcare Association and the Berkeley Haas Tech Club, and sponsored by Google.
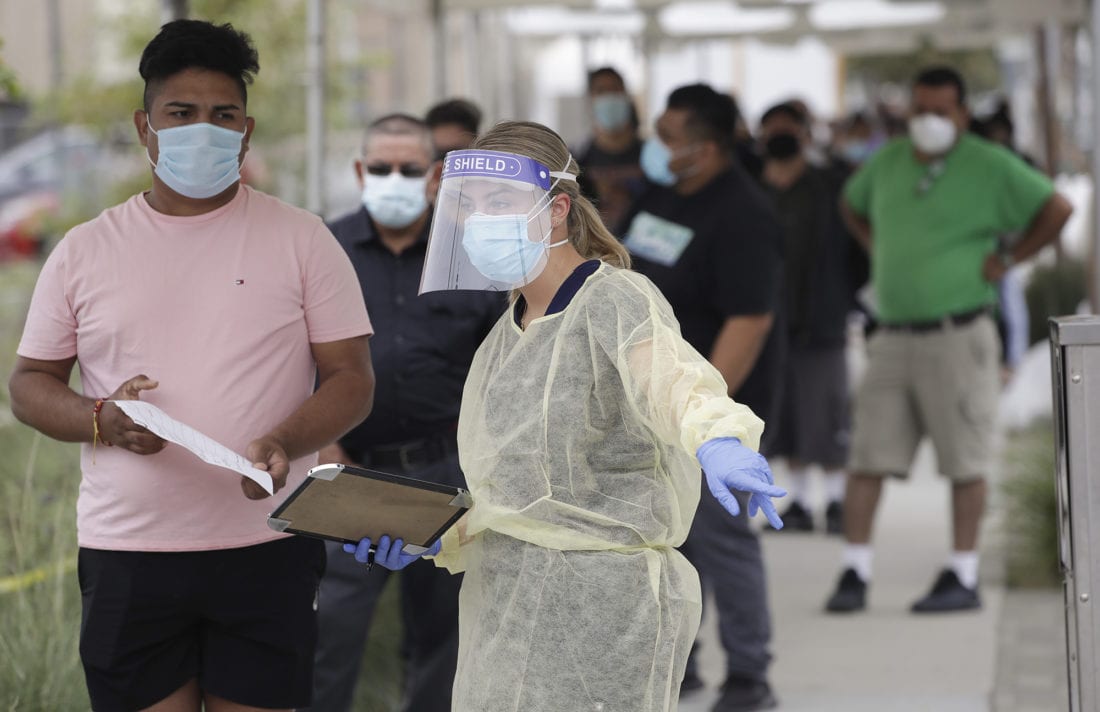
For the competition, students were asked to come up with an innovative solution to address mental health issues in the construction industry, which reports some of the highest rates of depression and suicide.
Team CLiKS pitched a mental health app that addressed three critical factors: prevention, assessment, and intervention. Through this app, construction workers would have access to music, podcasts, mental health specialists, peer volunteers, and a community-based forum to seek emotional support. The app would also collect daily mental health data from users through notifications, wellness checks, and diary entries.
The team credited its success to interviewing and surveying more than 90 construction workers, powerful storytelling, and a personal commitment to helping construction workers with mental health issues–an issue that hits close to home for Chen, Kim, and Li.
Chen, a civil engineer who’s worked in the construction industry, said one of her co-workers committed suicide. “The amount of work, the physical stress, and the financial instability that comes with the job pushes people to the edge.”
Kim, an Army veteran, said several soldiers he served with had committed suicide and Li, a music rehabilitation therapist, treats patients with severe mental health illnesses.
Su said the cause was important to him and he wanted to leverage his AI and computer engineering skills to help.
The team also credited its success to their construction industry mentor Matt Schulte; Rebecca Portnoy, a professional faculty member who teaches an organizational culture course called Leading People; and James Sallee, an associate economics professor at UC Berkeley.
“As a first-year Evening and Weekend MBA student without previous business knowledge, I was thankful to have taken a class with Prof. Sallee to guide my thinking and to tackle this mental health challenge from a health and business perspective,” Li said.
 Before Berkeley Haas’ dual-degree Biology+Business program even launched, junior Michelle Podlipsky attended a biotech seminar hosted by program planners and knew she’d found her calling.
Before Berkeley Haas’ dual-degree Biology+Business program even launched, junior Michelle Podlipsky attended a biotech seminar hosted by program planners and knew she’d found her calling.