Topic: Healthcare
First winners of Baillie Gifford-backed Panmure House Prize into breakthrough innovation announced
Carlos Orellana, MBA/MBH 10
CEO and Co-Founder, salauno

A decade ago, Carlos Orellana and friend Javier Okhuysen took on one of Mexico’s biggest health crises: blindness. Loss of sight—often from cataracts—is the country’s second-leading cause of disability, according to the World Bank Group’s International Finance Corporation. But the public health system has a years-long waitlist for cataract surgeries.
Their company, salauno, provides comprehensive eye care to anyone in Mexico, regardless of income. They modeled it after a nonprofit in India that performs affordable cataract surgeries for low-income patients—a success built around high-volume, high-quality care and efficiencies via technology, a hub-and-spoke patient referral network, and a vertically integrated supply chain. Orellana and Okhuysen saw an opportunity to complement this model with private investment and digital marketing to build a for-profit company.
The pair opened their first clinic in 2011 and had positive cash flow within two months, eventually serving some 250,000 patients annually at 27 clinics located in easily accessible retail locations. By 2020, salauno’s independent-contractor doctors were performing about 800 cataract surgeries a month—four to five times the rate of the average ophthalmologist and at 30–40% below private market rates. Orellana and Okhuysen began eyeing other Latin American markets.
Then the pandemic forced a restructuring that in hindsight, Orellana says, was overdue. They refocused their resources on high-potential services and closed seven under-performing clinics. They also introduced agile sprints to better prioritize and adapt to business shifts. This spring, business rebounded to 108% of pre-COVID, same-clinic volume. “In many ways, we’re stronger today—more focused and more nimble,” says Orellana. Talk about vision.
Berkeley startup aims to be a game changer in autoimmune disease therapy
Elle Wisnicki, MBA 22: Why goats should be part of mental healthcare
Haas Voices is a first-person series that highlights the lived experiences of members of the Berkeley Haas community
Elle Wisnicki, MBA 22, dreams of opening a wellness retreat center that offers animal-assisted therapy to children and adults—and she’s moving closer toward that goal at Haas. Wisnicki is a 2021 recipient of the John E. Martin Fellowship, (named for the father of Michael Martin, MBA 09) awarded to students who are working to improve mental healthcare quality and access.

I’m Black and Jewish and was raised by a single mom. I was an independent kid, always wanting to help others, so when I wasn’t caring for stray animals in the neighborhood, you could find me babysitting.
Growing up in Hollywood, Calif., where wealth exists parallel to a large population experiencing homelessness, I learned about mental health challenges at a young age. My mom and I got to know the stories of our neighbors who were homeless and faced post-traumatic stress disorder (PTSD), schizophrenia, depression, and more.
From childhood to high school, my career aspiration was to become an OB/GYN doctor or genetic counselor for families. However, after realizing that a lot of people can’t even get to the doctor for basic care, I shifted my goals away from providing care to helping people access care.
After realizing that a lot of people can’t even get to the doctor for basic care, I shifted my goals away from providing care to helping people access care.
After undergrad at Columbia University, I worked in consulting. At that job, I began connecting the dots among common mental health issues within different groups of people I’d met and worked with for over a decade, including homeless veterans, patients I worked with at Planned Parenthood, students I supported as an RA in my dorm, and even my financially well-off consulting coworkers who were burning out. No matter their walk of life , many shared a common thread: determining how to best address their mental health problems.
When I started putting it all together I began to see how I could thrive in this line of work and I wanted to start focusing on it right away. When I considered leaving consulting, I knew I had to align my career with my values so that my work would reflect my life’s greater purpose. After reaching out to diverse people in my network, I was inspired to become a mental health coach at Sibly, a text-based mental health and wellness app.
This was the first step toward starting my own mental health-related venture. However, I knew that creating a startup without the support of an MBA network would be challenging. So I initially came to Haas to focus on startup solutions for crisis response. What I quickly learned was that the many hours of research, customer discovery calls, and networking on a computer screen, on top of my MBA lectures, was leading to burnout.
In November 2020, I took the month off of my startup to spend some time restoring my own mental health. I volunteered for a ferret rescue and took llamas on walks up north in Yuba City, played with goats and did goat yoga in Half Moon Bay, and worked with kitten rescues. My soul lit up.
My soul lit up. I felt healed when an animal rested in my lap or greeted me.
I felt healed when an animal rested in my lap or greeted me, or when I moved my body around innocent beings, who only wanted to provide affection.

I realized others enjoy animals and nature in a healing way as do I and many people are looking for alternative wellness solutions. My potential customers told me they benefited from being closer to nature, but craved structure and couldn’t find affordable group wellness centers near them.
My vision is to offer that structure, by opening a retreat center with half day, full-day, and weekend wellness retreats. I’m also considering animal-assisted individual and group therapy, goat yoga, sustainable farming workshops, garden box subscriptions, children’s birthday parties, summer camps, a petting zoo, products, and transportation to access all of these services through bus rides between San Francisco and Oakland.
When I was applying for the Martin fellowship I connected with a Haas alum who had won a similar fellowship a few years before me. We recognized we both had similar goals. He recently began developing land he and his family own and considering what kind of venture they want to use it for. We’ve started discussions around the types of pilots we will put together to determine what is most appealing to our customers.
In addition to these plans, I continue to work in mental health tech. This semester, through the Lean Launchpad entrepreneurship class, I worked for a wellness startup Shimmer, focused on employer wellness benefits and insurance. My summer internship is focused on health insurance and mental health access for children and youth in foster care.
Throughout this journey, I’ve realized how grateful I am to be living and working at a time where as a society we’re finally prioritizing mental health. There has been tremendous growth in the wellness industry and I am thrilled about increasing access and with the movement toward mental health destigmatization.
Biggest health insurer plans to deny ER bills if it doubts you had an emergency
Fahed Al-Essa of Mayv: How anyone can build habits for optimal wellness, performance, & focus
Lean management associated with positive hospital performance
Can’t book a vaccine? These Berkeley students want you to call their hotline
Health Influencers
Haas alumni accelerate healthcare’s future
For 200 years, the stethoscope has been the workhorse of physical exams. But a stethoscope is only as good as the human ear listening to it. How could it be adapted for the digital age? wondered Jason Bellet, BS 14, and two Berkeley friends: Connor Landgraf, BS 13, MEng 14 (bioengineering), and Tyler Crouch, BS 14 (mechanical engineering).
In 2013, the trio co-founded Eko Devices and, with support from Berkeley’s SkyDeck Accelerator Program, developed a $349 stethoscope that can amplify heart and lung sounds 40 times better than its analog cousin. Connected software generates sound waveforms and electrocardiograms that allow some 80,000 clinicians to “see what they hear” and share recordings as needed. Last fall, the Oakland-based company, with 115 employees, closed on $65 million in Series C funding and partnered with AstraZeneca to develop new screening tools.

“Heart disease is the No. 1 killer worldwide, and there are millions of people with undiagnosed cardiac problems that can now be detected with greater accuracy in 45 seconds during a routine checkup,” says Bellet (shown right). Early last year, the FDA cleared Eko’s algorithm for detecting heart murmurs and atrial fibrillation; a separate algorithm received an FDA emergency use authorization to help clinicians detect a weak heart pump in COVID-19 patients, an especially high-risk group.
Today, Eko is more than a device maker. It’s a software and data-science company aiming to develop artificial intelligence-powered screening tools that can detect a range of health conditions in 60 seconds during a routine checkup, says Bellet. His team is also building a virtual primary care platform.
Haas community healthcare innovations like Eko are booming. From startups to Fortune 500 companies, venture capital firms to nonprofits, alumni are leading monumental shifts in healthcare—often backed by huge sums of money. Some entrepreneurs, like Bellet, are focused on improving preventative care and disease diagnosis or helping to develop new drugs and treatments. Others are working to streamline features of healthcare that often hinder innovation: payment models, organizational structures, and regulations. In interviews, Haas alumni reveal a shared mission: to make medical care—a $3.8 trillion business in the U.S. in 2019, according to the Centers for Medicare & Medicaid Services—more affordable, accessible, and scalable.
Using ‘real-world’ data
In Ohio’s Montgomery County, death rates from opioid overdoses have been among the nation’s highest and are surging anew amid the pandemic. It’s also the test site for an ambitious effort by Alphabet-owned Verily Life Sciences to reinvent addiction treatment and recovery. Called OneFifteen—named for the country’s average daily opioid death rate of 115 people in 2017—it features state-of-the-art medical and residential facilities on a 4.5-acre campus in Dayton.

Treating substance abuse, with its sky-high relapse rates, is difficult for many reasons, says Rebecca Messing Haigler, MBA/MPH 09, Verily’s health economics lead and recently announced chief development officer of portfolio company Onduo. Doctors lack high-quality information about how different patients respond to various treatments, and little or no coordination exists among clinicians, communities, and families. Payment models are also broken, she says. Patients don’t receive the comprehensive care they need in part because insurers typically pay for services up front—not based on outcomes.
OneFifteen’s model, which Messing Haigler helped design, relies on a comprehensive care continuum powered by a technology infrastructure that enables better data collection throughout the treatment and recovery process, from data sources including state and county programs, mobile apps, family surveys, employer updates, and the criminal justice system, among others.
“When patients fall off the radar, we can find out what happened from families or the community or if they showed up for work from employers,” says Messing Haigler. This could lead to improvements in treatment and at a faster rate.
Messing Haigler is describing a relatively new phenomenon in healthcare known as “real-world” data. The term essentially refers to the multitude of health-related information generated outside of a doctor’s office. Think voluntary user health surveys, fitness trackers—even insurance claims. Verily’s mission is to combine this data (with member consent and rigorous privacy policies) with machine learning to better prevent, detect, and manage diseases. For Messing Haigler, it also means developing new economic models, including payment structures based on successful patient outcomes.
When patients fall off the radar, we can find out what happened from families or the community or if they showed up for work from employers.
Real-world data is a byproduct of the booming digital health market. Seed fund Rock Health estimates that venture capitalists poured a record $14 billion last year into U.S. digital health companies, a 72% jump from the previous peak in 2018. McKinsey & Company valued the global digital health market at $350 billion in 2019—before the pandemic.
 Terrell Baptiste, MBA 20 (shown right), thinks about real-world data and its promise in another context: clinical drug trials. Last year, he joined Gilead Sciences as a senior manager to identify ways the pharmaceutical company can use information from nontraditional sources to speed the development and approval of new cancer drugs. A 2016 federal law mandated that the FDA incorporate data from outside traditional clinical trials into its approval process for pre-market pharmaceuticals. It’s early days for the FDA-developed framework for using real-world data, but the impact will be revolutionary: Trials can take eight years or more to conduct and are limited in scope because they depend on volunteers—who are often white, educated, and retired.
Terrell Baptiste, MBA 20 (shown right), thinks about real-world data and its promise in another context: clinical drug trials. Last year, he joined Gilead Sciences as a senior manager to identify ways the pharmaceutical company can use information from nontraditional sources to speed the development and approval of new cancer drugs. A 2016 federal law mandated that the FDA incorporate data from outside traditional clinical trials into its approval process for pre-market pharmaceuticals. It’s early days for the FDA-developed framework for using real-world data, but the impact will be revolutionary: Trials can take eight years or more to conduct and are limited in scope because they depend on volunteers—who are often white, educated, and retired.
With the combination of real-world data and digital health technologies, such as smartphones, clinical-trial volunteers could participate from home, allowing for more frequent monitoring of a possible treatment and thus faster discoveries. FDA regulators could also monitor a drug’s effects over a longer period of time.
For Baptiste, using real-world data in clinical trials has another crucial advantage. Marginalized paitients—often an afterthought in healthcare generally, and drug development specifically—can participate in studies and benefit from new ways of working that have arisen from the pandemic.
“Clinical trials measure effectiveness at a specific point in time and for a patient population who may not be the only ones actually benefiting from it,” says Baptiste, whose work includes volunteer research on behalf of sickle cell disease patients, the majority of whom are African American. “Real-world evidence attempts to fill the large gaps in knowledge about who could benefit from a new treatment. I’m hopeful this will help usher in more effective, realistic, and diverse ways to conduct clinical trial research.”
Closing gaps in care
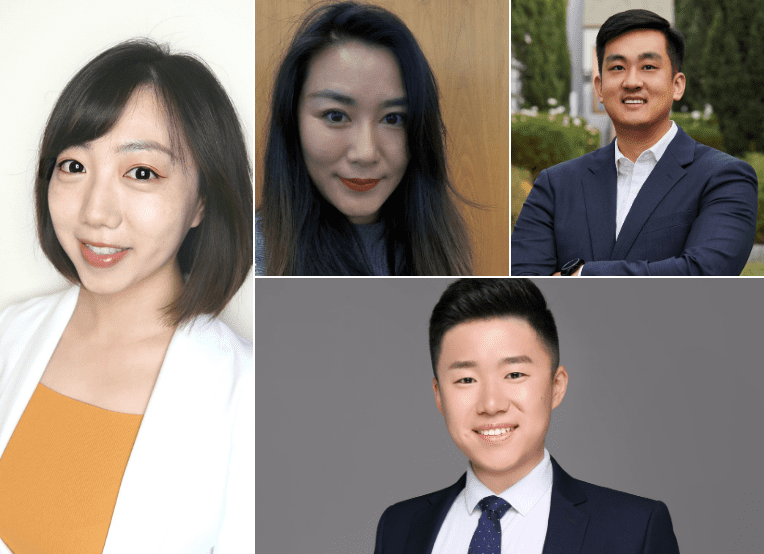
 Lauren Dugard Thomas, MBA/MPH 17 (shown left), works to address health inequities by improving the innovation process itself. At Blue Shield of California, where she’s a senior manager in enterprise innovation, she empowers all employees to generate entrepreneurial solutions, like with internal design challenges à la Shark Tank. She also ensures that underserved populations are factored into every business decision, big or small.
Lauren Dugard Thomas, MBA/MPH 17 (shown left), works to address health inequities by improving the innovation process itself. At Blue Shield of California, where she’s a senior manager in enterprise innovation, she empowers all employees to generate entrepreneurial solutions, like with internal design challenges à la Shark Tank. She also ensures that underserved populations are factored into every business decision, big or small.
Dugard Thomas says that for companies committed to reducing inequities, “the first step is educating internal decision makers about disparities and making it clear that maintaining the status quo will only widen the gaps.”
Since the increase in national awareness of racial injustice last summer, she’s seen a spike in LinkedIn job listings for experts in social determinants of health. Even so, Dugard Thomas says real change goes beyond budgets and head counts.
“It’s about the mindset, expectations, and practices of leaders at all levels of the organization,” she says. “Do you want to include more Black and brown individuals in program design? Great. How are you incentivizing that from a leadership standpoint?”
Supercharging blood tests
Colorectal cancer is the second-leading cause of cancer deaths in the U.S., yet one-third of adults age 50 to 75 don’t get screened, according to the Centers for Disease Control (CDC). Newer tests using stool samples collected at home haven’t changed this.

Atul Sharan, MBA 91, has a solution. His company, CellMax Life, has developed what he says is the first blood test for preventive screening for colon cancer—one that, according to a recent study conducted at Stanford’s Veterans Affairs Palo Alto Health Care System, successfully detects pre-cancerous polyps. It works by searching for extremely rare abnormal dysplastic epithelial cells and tiny traces of DNA that tumors shed. Other tests based on the company’s technology are already sold in Asia. CellMax plans to seek FDA approval before introducing the screening to the U.S. next year.
I’m hopeful [real-world evidence methods] will help usher in more effective, realistic, and diverse ways to conduct clinical trial research.
“The only real cure for cancer is early detection,” says Sharan, who started CellMax Life nearly a decade ago after his mother was diagnosed with late-stage, untreatable cancer and his wife with a malignant breast tumor shortly after being cleared by a negative mammogram. His company, which has raised more than $50 million, is part of a growing market for non-invasive “liquid biopsies” that use advanced genomic sequencing and machine learning to identify diseases and potentially tailor treatments to individuals. Bill Gates and Jeff Bezos, for example, poured over $100 million into liquid-biopsy company Grail, which sold last year for $8 billion.
Reinventing autism care
One in 54 children in the U.S. were diagnosed with autism in 2016, according to the CDC. Twenty years ago, it was just one in 150. No surprise, then, that waitlists for therapy can run up to six months.
Soaring demand for autism care isn’t the only problem, says Jia Jia Ye, MBA/MPH 11. Kids often need multiple forms of therapy—behavioral, speech, and physical—for up to 30 hours a week. Specialists often work independently, making it time-consuming and frustrating for parents to coordinate care and navigate labyrinthine insurance rules.

Ye’s groundbreaking solution is to combine expertise and payments at a single locale. A year ago, she co-founded Springtide Child Development with $18 million in Series A funding. Now with three clinics—two in Connecticut and one opening this summer in Massachusetts—the startup employs specialists from across disciplines, coordinates appointments, and handles insurance claims. Ye says consolidation enables an unprecedented degree of standardization in care.
Just as important: Ye and her team can quantify patient progress, which smaller operations can’t do for lack of money and data. “When you take an interdisciplinary approach to autism treatment, you see rapid improvement in kids’ progress,” says Ye. “And you can show it through consistent outcome metrics at all levels of care.”
Advancing women’s health
For Amy Fan, MBA/MPH 19, improving care is about making birth control more accessible and affordable for U.S. women—especially the 60% who are on Medicaid, uninsured, or underinsured—to get birth control. She co-founded Twentyeight Health in late 2018 to offer online reproductive services.
When you take an inter-disciplinary approach to autism treatment, you see rapid improvement in kids’ progress.
Her model is straightforward: Women complete an evaluation with a board-certified physician via a combination of asynchronous and live telemedicine—including phone and direct message—for a prescription for birth control pills, rings, patches, or shots. A monthly supply of pills starts at $18; for insured women, only co-pay fees (typically $0) apply. Twentyeight Health is the only online reproductive platform focused on underserved women, and it’s often the only player accepting Medicaid in the states where it’s active. It also partners with Bedsider’s Contraceptive Access Fund to provide a year of free birth control for uninsured women.

Twentyeight Health’s expansion has been gradual as the company navigates state-by-state Medicaid rules, but today, the company operates in nine states, including New York, North Carolina, and Florida. Last fall, the startup landed $5.1 million in seed funding.
“So much of healthcare is focused on people with a high ability to pay,” says Fan (shown right). “For low-income patients, and for women of color especially, we put so many burdens on them without trying to understand how we can make it easier for them to access healthcare.”
Powering innovation
Fan attributes much of Twentyeight Health’s success to networks of healthcare insiders—within Haas and beyond—who have offered advice and opened doors.
 They include Juan José Orellana, BS 95 (shown left), a Los Angeles-based strategy consultant who’s held senior roles within startups and the Fortune 200 company Molina Healthcare. He helped Fan explore the potential of expanding Twentyeight Health through partnerships with payers and providers.
They include Juan José Orellana, BS 95 (shown left), a Los Angeles-based strategy consultant who’s held senior roles within startups and the Fortune 200 company Molina Healthcare. He helped Fan explore the potential of expanding Twentyeight Health through partnerships with payers and providers.
“To innovate in healthcare, you need to be part of an ecosystem,” Orellana says. “You need to be able to tap into a value network that can facilitate collaboration, accelerate learning, and provide matchmaking for your organization’s needs and offerings.”
 Indu Subaiya, MBA 06 (shown right), has made a career out of fostering ecosystems in healthcare. First as a co-founder of Health 2.0 and now as president of Catalyst @ Health 2.0, she’s organized conferences, open-innovation challenges, and pilot programs to introduce new ideas to deep-pocketed stakeholders. Too often, she says, healthcare entrepreneurs can’t get the traction to scale up. “My primary mission is to introduce groundbreaking technology to the world,” she says.
Indu Subaiya, MBA 06 (shown right), has made a career out of fostering ecosystems in healthcare. First as a co-founder of Health 2.0 and now as president of Catalyst @ Health 2.0, she’s organized conferences, open-innovation challenges, and pilot programs to introduce new ideas to deep-pocketed stakeholders. Too often, she says, healthcare entrepreneurs can’t get the traction to scale up. “My primary mission is to introduce groundbreaking technology to the world,” she says.
In the last 15 years, Subaiya’s conference platform has debuted hundreds of startups, including Teladoc, a big provider of telehealth services, and Livongo Health, which helps patients manage diseases digitally. Last year, Teladoc bought Livongo for $18.5 billion. She and her team have also coordinated more than 90 contests, with $9 million in total prize money.
One competition, worth $100,000, drew scientists from 18 countries in a race to build a better COVID outbreak prediction model using government data and millions of Facebook user surveys tracking virus symptoms. The CDC has incorporated the winning model, developed by a Georgia Tech team, into its pandemic forecasting—and found it to be among the top five most accurate prediction tools. “That’s a phenomenal example of open innovation,” says Subaiya.
Innovation, accessibility, scaling up—just as in medicine, different balms can help to heal our healthcare system. And the Berkeley Haas community is shaping countless paths to greater wellness for everyone.
Researchers publish recommendations for using behavioral science to increase vaccine uptake
Moving the middle: How to get more people to take vaccines
Experts explain why Johnson & Johnson and Merck collaboration will change vaccine rollout
Haas Healthcare Conference to explore COVID-19 response, racial equity
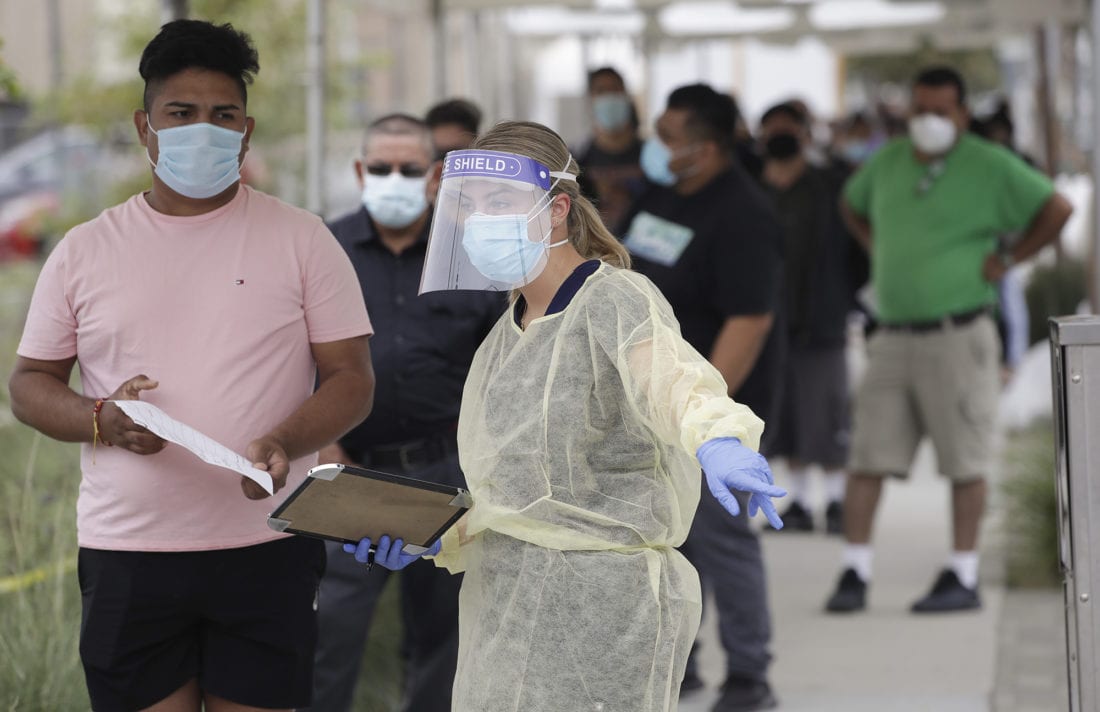
Innovative COVID-19 testing methods, digital options for mental health treatment, and racial equity challenges in healthcare are among the topics to be explored during the 2021 Haas Healthcare Association Conference.
With a theme of “Finding New Breath: Emerging Stronger Through Health Crises,” the 14th Annual Haas Healthcare Association Conference will be held online from Feb. 22-24. The conference, typically held at UCSF Mission Bay on a Friday, will span three half-days.

This year’s theme is a nod to the many challenges that have impacted breathing over the past year—from the COVID-19 pandemic to rampant wildfires, said conference co-chair Corrine Marquardt, MBA/MPH 21. “2020 was so hard, with many challenges focused around mental and physical health, so we wanted this year to be about resilience and coming through stronger than we were pre-crises,” she said. “We also wanted to address how tech and innovation can help get us through our health challenges.”
Each day will focus on a different theme, including health and environmental equity, (day one) COVID-19 & pandemic response, (day two) and health technology & innovation (day three). A career networking night is planned on Monday, Feb. 22, from 4-5 pm.
“We have a lot of ground to cover over three days and we’ve brought together some of the brightest minds in this space to reflect on everything from racial injustice in healthcare to vaccine development and distribution challenges,” said conference co-chair Ben Delikat, MBA/MPH 21.
Berkeley Haas Dean Ann Harrison and Michael Lu, Dean of UC Berkeley’s School of Public Health, will welcome attendees to the conference, which includes many guests from across the UC Berkeley campus.
We wanted this year to be about resilience and coming through stronger than we were pre-crises. —Corrine Marquardt.

Monday’s line-up includes Dr. Alice Chen, Chief Medical Officer for Covered California, as well as two panels on health equity, one focused on health equity implications of COVID-19 and the other focused on addressing social determinants of health through payers and providers.
Tuesday session highlights include a climate-change focused conversation with Kristine Belesova, deputy director of the Centre on Climate Change and Planetary Health at the London School of Hygiene, along with a COVID-19-focused conversation with Niranjan Bose, managing director of Health & Life Sciences Strategy at Gates Ventures.
Dr. Guy Nicolette, assistant vice chancellor, University Health Services (UHS) of UC Berkeley will join Dr. Anna Harte, UHS Medical Director of UC Berkeley, for a panel discussion with Othman Laraki CEO of genetic test company Color Genomics about public/private partnerships in addressing COVID-19.
On Wednesday, Alice Raia of KP Digital and Kim MacPherson, executive director of Health Management at Haas, will discuss recent digital transformation trends in health systems. The day also includes a conversation on how technology has enabled global health endeavors through COVID-19, as well as a panel on how technology solutions are being used to address mental health. Mariya Filipova, co-founder of the XPRIZE Pandemic Alliance and Anthem’s former vice president of innovation, will close the conference in conversation with Marquardt.
Business leaders from organizations including Google, Jazz Ventures, Headspace, Accenture, Vida Health, and UCSF will participate.
The conference is open to the public. Tickets are available here.
Study: Testing policies should vary based on demand to catch the most COVID-19 cases
NeuroBo Pharmaceuticals Acquires ANA Therapeutics for Late-Stage Oral Antiviral Development Program
Inside the collapse of a disrupter: How Haven’s high hopes of redefining health care came to a crashing halt
2020 in review: A year of “beyond yourself”
If ever there was a year that called on all of us to embody the Berkeley Haas Defining Leadership Principles, it was 2020. It so happened that this tumultuous year also marked the 10th anniversary of codifying these principles, which have become deeply embedded throughout our school over the past decade.
This year, many in our community went beyond themselves to help those struggling with pandemic impacts, while others questioned the status quo, speaking out against racial inequities and violence against Blacks and African Americans. Others showed confidence without attitude in sharing expertise and skills to help small businesses or solve other problems related to the pandemic. And we were all reminded to be students always as we adapted to life online.
While 2020 challenged us in many ways, it also taught us that a global pandemic can bring out the best in ourselves and our community, and there is a lot worth recognizing—and even celebrating—as the year comes to a close. Here’s what we’ll remember.
Black Lives Matter

As waves of protests swept the country in response to the murder of George Floyd, Breonna Taylor, and Ahmaud Arbery, Haas community members spoke out publicly about violence against Blacks and African Americans, sharing deeply personal narratives of anguish, frustration, and devastation. “If you read no further, understand this,” wrote Marco T. Lindsey, associate director of Diversity, Equity, and Inclusion at Berkeley Haas, in a widely shared letter to the community. ”Black Lives Matter = if anyone kills a Black person, their punishment should be the same as if they killed someone from any other race.” Responding to BLM, students, faculty, and staff rallied together, leaning on each other for support. They raised funds to rebuild damaged Black-owned businesses and for racial equity organizations, and embarked on personal journeys toward allyship through campus study groups, anti-racist challenges for students and staff, and “Ask Me Anything” sessions.
Students stepping up

Among the notable 2020 projects were the Berkeley Community Business Partnership, led by Lokilani Hunt, MBA 22. As president of the group, Hunt led 60 MBA students who worked with local community groups to offer consulting support to small Bay Area businesses. Their work ranged from organizing a worker-owned cooperative for struggling restaurants to developing new financing pipelines for women-owned businesses to helping small grocers build their online presence and upgrade their payment systems. The effort builds on a project launched last spring by the Sustainable and Impact Finance (SAIF) initiative at Berkeley Haas. Meanwhile, Peter Gallager, EWMBA 22, a member of the University Development & Alumni Relations fundraising team, helped raise $10 million in three weeks for a pop-up coronavirus testing lab at the Innovative Genomics Institute. Raising that kind of capital can take months or even years to accomplish in normal times. “I’ve never experienced anything like that, but these are unprecedented times and people are responding in unprecedented ways,” he said.
Janet Yellen nominated for Treasury Secretary

Berkeley Haas Prof. Emeritus Janet Yellen’s career has been brilliant, groundbreaking, and defined by a commitment to public service. Among her many accomplishments: She was the first woman to chair the Federal Reserve Board of Governors, she chaired the President’s Council of Economic Advisors, and she taught thousands of Berkeley Haas MBA and undergraduate students from 1980 to 2006. Now poised to become President-elect Biden’s lead economic advisor at one the nation’s most challenging periods, Yellen is expected to be a champion for all those facing the economic devastation of the pandemic.
Former Dean Laura Tyson, professor of the graduate school and her longtime close colleague, told the Financial Times that Yellen is driven by neither the “power” nor the “kudos” of the position. “She is doing it to serve the public, through the tools she has to understand economic issues.”
The passing of faculty greats
Nobel laureate Oliver Williamson, a pioneer of organizational economics, passed away on May 21 at age 87. Williamson, known to friends and colleagues as Olly, shared the 2009 prize in economics with political scientist Elinor Ostrom of Indiana University for his insight on the “make-or-buy”decision—the process by which businesses choose whether to outsource a process, service, or manufacturing function. “Williamson’s work permanently changed how economists view organizations,” said Prof. Rich Lyons, who was dean when Williamson won the Nobel. “Yet for all of his intellectual creativity, I most often think of Olly as a person who lifts others.”
Last month we also lost Prof. Emeritus George Strauss, who passed away Nov. 27 at age 97. An icon in the field of industrial relations who served as a professor from 1960 until 1991, Strauss helped establish Haas as an organizational theory powerhouse starting in the 1960s. He was a prolific researcher and top scholar of organizational behavior, unions, workplace participation, and comparative industrial relations.
The scramble to move online

On March 9, it was all-hands-on-deck after Chancellor Carol Christ announced the campus would suspend in-person classes to control the spread of the novel coronavirus. Haas had to move 270 classes online virtually overnight. Faculty members scrambled to adapt, with Haas Digital, graduate student instructors, and other staff working overtime to support them. Those with more experience online stepped up to help colleagues. The work continued all summer, as faculty and staff worked to re-imagine classes, learn online pedagogy, and pre-record asynchronous material, while Haas invested in new technology. Dean Ann Harrison commended the efforts. “After watching our faculty and staff move within 36 hours to online teaching when the coronavirus broke out, I believe there’s little that we can’t do virtually going forward.”
Financial creativity to save small businesses

The Haas School of Business and Berkeley Law came together to play a critical role in developing the State of California’s new fund to support small businesses devastated by the coronavirus pandemic. The California Rebuilding Fund, a new public-private partnership operated by the Governor’s Office of Business and Economic Development (GO-Biz), uses government capital to attract private lenders to offer low-interest loans to small businesses—particularly the smallest firms and entrepreneurs from communities that have been historically disenfranchised. Professors Laura Tyson and Adair Morse contributed their finance and policy expertise to the innovative design of the fund. “The state put many groups together to try to get the best of the best ideas,” said Morse, the Soloman P. Lee Chair in Business Ethics. “We all came together to try to optimize a plan for the people of California.”
Researchers contributing to pandemic knowledge
As the pandemic spread, many faculty members used their knowledge and research prowess to shed light on the growing crisis and to search for solutions. Associate professors Jonathan Kolstad and Ned Augenblick laid out a strategy for cheap, mass COVID-19 surveillance testing; Asst. Prof. Abhishek Nagaraj and a team of researchers across four universities built the interactive Reopen Mapping Project to show how different policies affect employment and the number of deaths from the virus; Prof. Pierre-Olivier Gourinchas examined which government policies were most effective in staving off small business bankruptcies in Europe; while Assoc. Prof. Luyi Yang analyzed the optimal way to prioritize who gets COVID tests. Many others generously shared their expertise with the media, wrote commentaries and op-eds, participated in panels and the “New Thinking in a Pandemic” series, and gave lessons on leading through crises for a Berkeley Executive Education video series.
New leaders and faculty
Haas had a banner year for welcoming new leaders to the Dean’s suite, including Loretta Ezeife, chief financial officer; Howie Avery, assistant dean for Development & Alumni Relations; Michele de Nevers, in the newly-created position of executive director of sustainability programs, and Michelle Marquez, assistant dean of Human Resources. On the faculty side, nine new professors, including five women, joined Haas. The diverse, international group hails from Italy, Argentina, France, China, Canada, and California.
Pride in our big wins

Alum Collin Morikawa, BS 19, stunned the golf world last August by winning the PGA Championship, making history as one of the tournament’s youngest winners. Highlights from our many student competitions this year include a FTMBA team win at the Berkeley Haas Spring 2020 Tech Challenge, and a first-place FTMBA finish at the inaugural Oxford Global Private Equity Challenge in March. Yashoraj Tyagi and Akshay Gupta, both MFE 20, took first-place wins in the Moody’s Analytics competition. And another team of MFE students won first place in the Citadel West Coast Datathon. Eugene Kim, Zhuoran Li, Zixuan Chen, and Chen Su, all EWMBA 23, won the inaugural John E. Martin Healthcare Tech Challenge.
Alumni and faculty also netted academic honors, including Matteo Maggiori, PhD 12, who won the Fischer Black Prize—joining previous winner Prof. Ulrike Malmendier as a recipient of the prestigious award for the top finance scholar under age 40. Prof. Martin Lettau won the 2019 Roger F. Murray Prize for outstanding research from The Institute for Quantitative Research in Finance (The Q Group). Prof. David Teece was inducted into the Thinkers50 Hall of Fame, joining management greats Peter Drucker, Clay Christenson, Michael Porter, and his long-time collaborator Ikujiro Nonaka, PhD 82; Teece was also recognized as the top-cited scholar in the field of business and management, while Prof. Ross Levine was No. 10 for economics. Asst. Prof. Ellen Evers of the Haas Marketing Group was recognized with the Carol D. Soc Distinguished Graduate Student Mentoring Award, UC Berkeley’s premier award for graduate mentorship. Prof. Annette Vissing-Jørgensen was honored by the Swiss Finance Institute with its Outstanding Paper Award 2019 for “The Impact of Pensions and Insurance on Global Yield Curves”.
Rankings recognition

All of our degree programs again ranked in the Top 10 this year. The EWMBA Program ranked #2 and the Full-time MBA Program ranked #7 in U.S. News & World Report’s 2021 Best Business Schools; U.S. News ranked the Undergraduate Program #3. The Executive MBA Program (EMBA) was #1 in the world, according to The Economist; and the Master of Financial Engineering (MFE) Program placed #1 in the TFE Times ranking. Haas continued to climb in the Corporate Knights Better World Ranking, ranking among the very top U.S. business schools for incorporating sustainability into its research and teaching.
Berkeley Haas team wins Mental Healthcare Tech Challenge
An AI-powered app aimed to help construction workers experiencing anxiety, depression, and suicidal thoughts netted a first place win at the first inaugural John E. Martin Healthcare Tech Challenge. The competition was held online Nov. 16-20.
The winning team, Team CLiKS, included Eugene Kim, Zhuoran Li, Zixuan Chen, and Chen Su, all EWMBA 23. The team competed against 11 other teams from top U.S. business schools, including Wharton, Harvard, Columbia, MIT Sloan, and Kellogg for $10,000 in prize money.
Another Haas team placed second, earning $4,000 in prize money for pitching a chatbot that could collect health data, such as sleep patterns and appetite, and recommend tele-health therapy and wellness ambassadors stationed at construction worksites.

Team members included Sophie Schonfeld, Ben Delikat, both MBA/MPH 21; Doug Pollack, MBA/MPH 20; and Vishalli Loomba, MD/MS 23.
The competition was organized by the Berkeley Haas Healthcare Association and the Berkeley Haas Tech Club, and sponsored by Google.
For the competition, students were asked to come up with an innovative solution to address mental health issues in the construction industry, which reports some of the highest rates of depression and suicide.
Team CLiKS pitched a mental health app that addressed three critical factors: prevention, assessment, and intervention. Through this app, construction workers would have access to music, podcasts, mental health specialists, peer volunteers, and a community-based forum to seek emotional support. The app would also collect daily mental health data from users through notifications, wellness checks, and diary entries.
The team credited its success to interviewing and surveying more than 90 construction workers, powerful storytelling, and a personal commitment to helping construction workers with mental health issues–an issue that hits close to home for Chen, Kim, and Li.
Chen, a civil engineer who’s worked in the construction industry, said one of her co-workers committed suicide. “The amount of work, the physical stress, and the financial instability that comes with the job pushes people to the edge.”
Kim, an Army veteran, said several soldiers he served with had committed suicide and Li, a music rehabilitation therapist, treats patients with severe mental health illnesses.
Su said the cause was important to him and he wanted to leverage his AI and computer engineering skills to help.
The team also credited its success to their construction industry mentor Matt Schulte; Rebecca Portnoy, a professional faculty member who teaches an organizational culture course called Leading People; and James Sallee, an associate economics professor at UC Berkeley.
“As a first-year Evening and Weekend MBA student without previous business knowledge, I was thankful to have taken a class with Prof. Sallee to guide my thinking and to tackle this mental health challenge from a health and business perspective,” Li said.