UC Berkeley researchers have developed a strategy to massively increase the scale and frequency of COVID-19 testing while drastically lowering costs. The key is to pool samples using machine learning algorithms to look for transmission patterns and predict risk.
Associate professors Jonathan Kolstad and Ned Augenblick of Berkeley Haas and Ziad Obermeyer of the School of Public Health laid out their strategy for reducing the cost of screening from $100-$200 per test to just $3-$5 per person per day in an MIT Technology Review article. It’s based on a National Bureau of Economic Research working paper they published this month, along with economics PhD student Ao Wang.
“In the absence of a vaccine, it’s impossible to control COVID-19 without knowing who is infected, and the way to do that is through frequent, mass testing,” Kolstad said. “Testing once a month is almost totally useless to stop the spread by asymptomatic people, who are transmitting nearly half of new infections.”
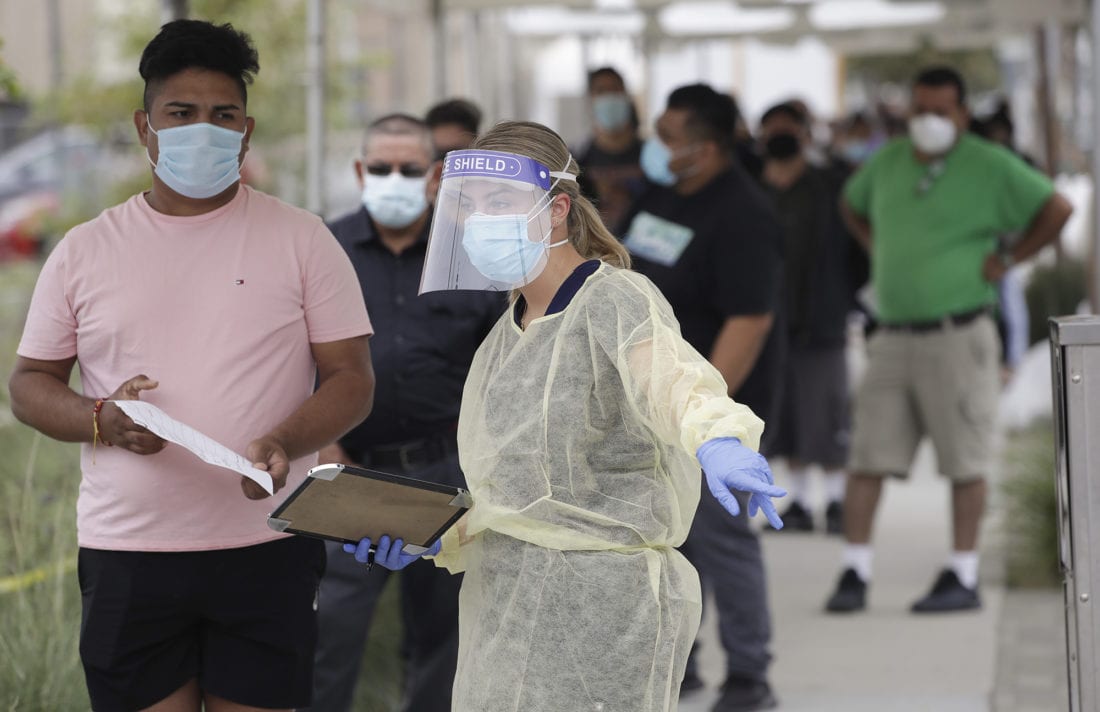
Testing capacity has been unable to handle the surge in new infections, with some results delayed by two weeks or more. To help reduce the strain, the U.S. Food and Drug Administration this month approved the use of pooled testing, in which multiple peoples’ samples are combined into one. If no virus is detected, the entire group is cleared with one test; if the virus is detected in the pool, however, each sample is tested individually to determine who is infected.
The method was first developed in the 1940s to test for syphilis, and the U.S. military uses the technique at its bases.
“Pooling would give us the capacity to go from half a million tests per day to potentially 5 million individuals tested per day,” Dr. Deborah Birx, a White House coronavirus task force official, told the American Society for Microbiology last month.
Pooled testing is far more efficient when the prevalence of the virus is lower, since fewer re-tests are required. But rapid changes in infection rates across geographic areas and disparate risks between groups of people—for example, health-care workers versus people working remotely—makes pooling a challenge to implement. That’s where the power of machine learning comes in, Obermeyer, Augenblick, and Kolstad write.
“Using publicly available data from employers and schools, epidemiological data on local infection and testing rates, and more sophisticated data on travel patterns, social contacts, or sewage, if available, modelers can predict anyone’s risk of having covid-19 on a day-by-day basis. This allows highly flexible approaches to pooling that drive huge efficiency gains,” they write.
In fact, the researchers determined that with efficient pooling of sample, more frequent testing actually drives down the number of tests needed—dramatically reducing the cost. It also reduces the spread of the virus. “According to our analysis, testing daily costs only twice as much as testing monthly. And daily testing can actively suppress the virus, whereas monthly testing really only allows us to see how badly things have gone.”
The technique would work particularly well on college campuses, nursing homes, or warehouses and factories—locations where a specific population of people interact frequently, Kolstad said. Even if the prevalence of the virus is initially high, those who are infected can quickly be identified through an initial screening, followed by pooled testing to quickly identify any new outbreaks.
The researchers acknowledge that there are logistical challenges to putting high-frequency pooled testing into practice, but that they can be solved—particularly as less-invasive tests, such as the saliva test now undergoing a trial at UC Berkeley, come online.
“Pooled testing that harnesses the power of machine learning makes paying the associated costs not only viable but, when weighed against the alternative of prolonged closures, a tremendous deal,” they write.